Australia: This is not a drill - Five reasons why the experts are worried about the next pandemic

By Ali Moore
Earlier this year, the World Health Organisation (WHO) issued a global alert for a disease that doesn’t exist yet. A potentially savage pathogen called Disease X.
“History tells us that it is likely the next big outbreak will be something we have not seen before,” says WHO committee science adviser John-Arne Rottingen.
By officially designating an unknown pathogen as a likely cause of a global outbreak, the WHO has upped the ante on the need to be better prepared.
While we may not know what ‘Disease X’ is, in all probability it’s coming. Conditions are ripe for its arrival.
But are we ready? Here’s five reasons why we should answer that question carefully.
1. The number of diseases is increasing
In May of this year in a Washington ballroom, a novel parainfluenza virus was unleashed on the world. It spread rapidly from person to person through coughing, and killed 20 per cent of those it infected. The first vaccine failed, and within a year 150 million were dead.
That was the hypothetical scenario , run by the Johns Hopkins Center for Health Security, to pinpoint the challenges the US and the world would face in the event of a truly devastating outbreak. Their virus was manmade, a bio terrorist attack on the world.
Closer to home, the Doherty Institute in Melbourne unleashed its own novel pathogen that spread from a music festival in regional Victoria to the rest of the country.
Preparing for the worst possible scenario is high on many agendas around the world - spurred on by a widely held understanding that the next pandemic is a case of when, not if.
Researchers have found both the number of outbreaks of infectious diseases and the types of diseases have increased in recent decades, with the number of outbreaks per year more than tripling since 1980.
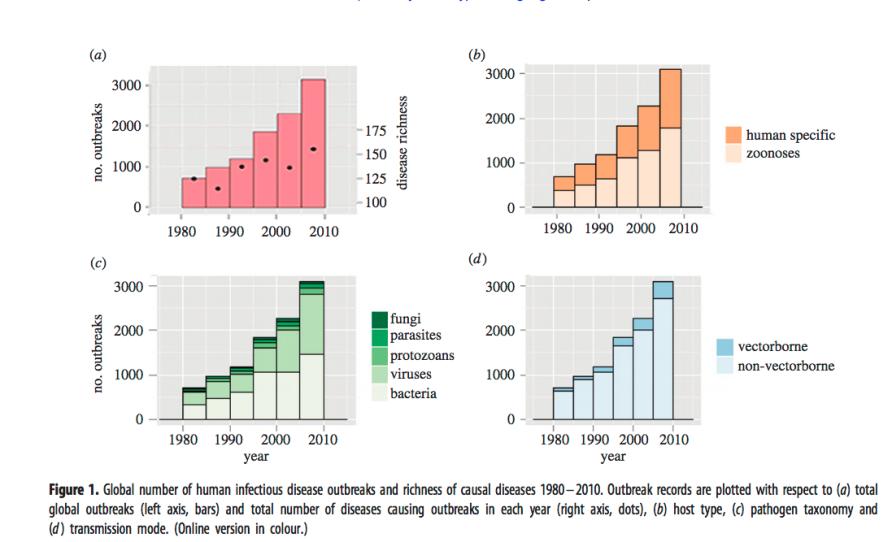
The number and types of infectious diseases have increased in recent decades. Picture: The Journal of the Royal Society
And infections are easily spread in a world of rapid urbanisation, warmer climates and persistent poverty. As well, the human race moves around a lot. With 4 billion passengers travelling by air last year alone, it’s not hard for a virus to hitch a ride and become a global problem.
Certainly diagnostics and surveillance have improved dramatically. But with an ever expanding catalogue of diseases, keeping watch is a complicated task.
There’s Ebola, SARS, Swine Flu and MERS ... or the Zika, Marburg, Nipah and Hendra viruses. Many of them are well established on the World Health Organisation’s priority disease list.
Now the officially designated ‘Disease X’ has been added to that list for the first time, the reality of an unknown pathogen as the potential cause of the next pandemic has taken on a new urgency.
The more diseases out there, the higher the risk one will become a global killer.

Air transport and passengers carried. Picture: World Bank
2. One of the biggest threats is constantly reinventing itself
One hundred years after the Spanish Flu infected up to a third of the world’s population, an unknown strain of influenza is widely seen as the most likely cause of the next pandemic. And for good reason.
The flu virus is constantly changing, which is why the seasonal flu vaccine has to be updated every year. It’s that constant morphing that poses the biggest risk.
For example, two of the most concerning strains of avian influenza currently kill up to 60 per cent of the people they infect. But what they can’t do is spread easily from person to person, only from bird to person. If that changes, all bets are off.
The very fact influenza does shapeshift, means there’s little incentive for drug companies to pour billions into researching and stockpiling vaccines. And so the hunt is on for a universal flu vaccine that would protect against most strains.
But, according to the Institute for Disease Modelling, if a newly emerged airborne pathogen started in South East Asia today, nearly 33 million people would likely be dead in just six months.
3. We are prepared - but what does that mean?
Australia has a pandemic preparedness plan, the Australian Health Management Plan for Pandemic Influenza, that runs to 232 pages.
It talks about the steps our health sector would consider taking in response to a pandemic, with a focus on flexibility. But it’s necessarily vague, and focusses more on process than exactly what would happen in practice, with too many unknowns to lock down an action plan.
And there are so many questions.
A ‘consistent communications strategy’ is key, but how does that happen when every state and territory leader, hospital, local GP, even local council health centre, will be called on for advice and counsel in the face of a pandemic emergency?
And what about decisions on when to close borders, shut schools, quarantine people and ration supplies? Or the vital question of who would get the first doses of a custom-made vaccine?
The plan simply notes that the “actual priority groups will need to be finalised in the light of the epidemiology of the pandemic virus”. It’s obvious that a plan on paper is exactly that until it’s really tested.
4. How confident is your local GP?
Imagine there is a pandemic declared: who would you turn to for advice and care?
A hastily set up flu clinic where you could well end up in a waiting room with other sick people, a health minister from a political party you may or may not trust, or your local doctor?
GPs would be at the front line - and unless things work differently to how they unfolded during the most recent Australian pandemic of Swine Flu in 2009, that could prove challenging.
Nine years ago, the north east of Melbourne was one of the hardest hit areas in Victoria. Local GP Dr Peter Eizenberg wrote a scathing rundown of his experience in the Medical Journal of Australia.
There were administrative burdens, laboratory test delays and a lack of clear communication. He says when the government changed its policy on Swine Flu, GPs were unsure whether to check websites or wait for faxes or letters from Chief Health Officers.
And his clinic received just a fraction of the personal protective equipment requested from the national stockpile, including just 40 per cent of goggles, six per cent of gloves and no masks.
Dr Eizenberg concludes: “It is only due to the low virulence of the virus that this pandemic has merely stressed our local service delivery and not completely paralysed both our and the statewide response.”
The government’s pandemic plan referred to above, has been rewritten since 2009, to allow for a “flexible and scalable” response. But the role of GPs appears to be largely covered by references to “other health sector stakeholders”, and not all GPs are confident the system will work better if it’s really pushed to the limit.
Supply issues with this year’s seasonal flu vaccine have not boosted confidence.
5. Australia has no national centre for disease control
Australia is the only country in the OECD that doesn’t have a national coordinating body responsible for communicable disease threats.
The US, the UK, Canada and the EU all have one. In our part of the world so does China, Cambodia, Japan, Thailand and Vietnam.
Nor are we among the 100 strong members of the International Association of National Public Health Institutes, which is designed to link and strengthen government health authorities in member countries.
There’s no question Australia does have a multiplicity of agencies and expert groups focussed on infectious diseases, but as the Australian Medical Association puts it, “the current approach to disease threats, and control of infectious diseases, relies on disjointed State and Commonwealth formal structures, informal networks, collaborations, and the goodwill of public health and infectious disease physicians.”
The call for an Australian CDC (the US Centre for Disease Control and Prevention) has been rejected by the government.
But advocates point to Canada’s experience with SARS. It was hit hard by the disease, with more than 40 deaths and an official cost of close to a billion Canadian dollars. An official review found poor coordination and inconsistent policies because there was no central governing body. As a result, there’s one now.
Many in the field hope it doesn’t take an experience like that for Australia to follow suit.